Artificial limb

An artificial limb is a type of prosthesis that replaces a missing extremity, such as arms or legs. The type of artificial limb used is determined largely by the extent of an amputation or loss and location of the missing extremity. Artificial limbs may be needed for a variety of reasons where a body part is either missing from the body or is too damaged to be repaired, including disease, accidents, and congenital defects. A congenital defect can create the need for an artificial limb when a person is born with a missing or damaged limb. Prosthetics are however not needed in the event of an accident where only the nerves were damaged and not the extremeties. In this case, Functional Electrical Stimulators (FES) are used.[1] [2] Industrial, vehicular, and war related accidents are the leading cause of amputations in developing areas, such as large portions of Africa. In more developed areas, such as North America and Europe, disease is the leading cause of amputations.[3] Cancer, infection and circulatory disease are the leading diseases that may lead to amputation.[4]
Contents |
History

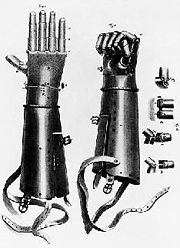
An artificial limb is mythologically referred to in the Rigveda, the "iron leg" given to Vishpala by the Ashvins. The first specimen discovered archaeologically, known as the Roman Capua Leg, was found in a tomb in Capua, Italy, dating to 300 BCE, and was made of copper and wood.[5] Roman bronze crowns have also been found, but their use could have been more aesthetic than medical[6]. Two artificial toes found on Egyptian mummies are even older, dating to 1295–664 BCE; these are being tested (as of July 2007) to determine whether they could have been used in life.[5] Armorers in the 15th and 16th centuries made artificial limbs out of iron for soldiers who lost limbs. Over the next several centuries, craftsmen began to develop artificial limbs from wood instead of metal because of the lighter weight of the material.
In the 19th century, limbs became more widespread due to the large number of amputees from wars such as the Napoleonic Wars in Europe and the American Civil War. An artificial leg designed by London’s James Potts in 1800 and patented in 1805 became known as the Anglesey Leg. The prosthetic was named after the Marquess of Anglesey who had lost his leg at Waterloo. James Potts fitted his prosthetic leg consisting of a wooden shaft and socket, steel knee joint, and an articulated foot with artificial cords or catgut tendons that connected knee flexion with foot flexion. The Anglesey Leg technology was brought to the United States in 1839 and became known as the American Leg. During the American Civil War, a Confederate soldier, J.E. Hanger, who had himself suffered the war's first amputation (see Battle of Philippi) founded what was for a time the world's largest artificial limb factory.
In England, Marcel Desoutter who was fitted with a wooden leg after an aviation accident, and his brother Charles, designed the first light metal limb to be manufactured. Their jointed Duralumin alloy leg was half the weight of the standard wooden leg. Developments included a frictional knee control, which allowed the wearer to control the speed and length of step, and the Desoutter cushion-joint foot, which imitated the natural action of the human foot. Desoutter Brothers, manufacturers of artificial limbs, was established in 1914 in London.[7]
Technology improved primarily for two reasons: the availability of government funding and the discovery of anesthetics. After World War II, the Artificial Limb Program was started in 1945 by the National Academy of Sciences. This program helped improve artificial limbs by promoting and coordinating scientific research on prosthetic devices.
In recent years, a great deal of emphasis has been placed on developing artificial limbs that look and move more like actual human limbs. Advances in biomechanical understanding, through the combined work of doctors and engineers, the development of new plastics, and the use of computer aided design and computer aided manufacturing have all contributed in the development of more realistic artificial limbs.[4][8]
Lower extremity prosthetics
Lower extremity prosthetics describes artificially replaced limbs located at the hip level or lower. The two main subcategories of lower extremity prosthetic devices are 1.trans-tibial (any amputation transecting the tibia bone or a congenital anomaly resulting in a tibial deficiency) and 2.trans-femoral (any amputation transecting the femur bone or a congenital anomaly resulting in a femural deficiency). In the prosthetic industry a trans-tibial prosthetic leg is often referred to as a "BK" or below the knee prosthesis while the trans-femoral prosthetic leg is often referred to as an "AK" or above the knee prosthesis.
Other, less prevalent lower extremity cases include the following:
- Hip disarticulations - This usually refers to when an amputee or congenitally challenged patient has either an amputation or anomaly at or in close proximity to the hip joint.
- Knee disarticulations - This usually refers to an amputation through the knee disarticulating the femur from the tibia.
- Symes - This is an ankle disarticulation while preserving the heel pad.
Lower extremity modern history
Socket technology for lower extremity limbs saw a revolution of advancement during the 1980s when Sabolich Prosthetics, John Sabolich C.P.O., invented the Contoured Adducted Trochanteric-Controlled Alignment Method (CATCAM) socket, later to evolve into the Sabolich Socket. The advancement was due to the difference in the socket to patient contact model. Prior, sockets were made in the shape of a square bucket with no specialized containment for either the patient's bony prominences' or muscular tissue. Sabolich's design held the patient's limb like a glove, locking it into place and distributing the weight evenly over the existing limb as well as the bone structure of the patient. This was the first instance of ischial containment and led to an extreme advancement in patient accomplishment. Because of Sabolich's dedication to research and development in lower extremity prosthetics, Sabolich Prosthetics saw the first above the knee prosthetic patients walk and run step over step with both one leg and two legs missing, walking down stairs, suction sockets, modern plastic and bio elastic sockets, sense of feel technology, and numerous other inventions in the prosthetic field.
Types

There are four main types of artificial limbs. These include the transtibial, transfemoral, transradial, and transhumeral prostheses. The type of prosthesis depends on what part of the limb is missing.
Transtibial Prosthesis
A transtibial prosthesis is an artificial limb that replaces a leg missing below the knee. Transtibial amputees are usually able to regain normal movement more readily than someone with a transfemoral amputation, due in large part to retaining the knee, which allows for easier movement. In the prosthetic industry a trans-tibial prosthetic leg is often referred to as an "BK" or below the knee prosthesis.
Transfemoral Prosthesis
A transfemoral prosthesis is an artificial limb that replaces a leg missing above the knee. Transfemoral amputees can have a very difficult time regaining normal movement. In general, a transfemoral amputee must use approximately 80% more energy to walk than a person with two whole legs.[9] This is due to the complexities in movement associated with the knee. In newer and more improved designs, after employing hydraulics, carbon fibre, mechanical linkages, motors, computer microprocessors, and innovative combinations of these technologies to give more control to the user. In the prosthetic industry a trans-femoral prosthetic leg is often referred to as an "AK" or above the knee prosthesis.[10]
Transradial Prosthesis
A transradial prosthesis is an artificial limb that replaces an arm missing below the elbow. Two main types of prosthetics are available. Cable operated limbs work by attaching a harness and cable around the opposite shoulder of the damaged arm. The other form of prosthetics available are myoelectric arms. These work by sensing, via electrodes, when the muscles in the upper arm moves, causing an artificial hand to open or close. In the prosthetic industry a trans-radial prosthetic arm is often referred to as a "BE" or below elbow prosthesis.
Transhumeral Prosthesis
A transhumeral prosthesis is an artificial limb that replaces an arm missing above the elbow. Transhumeral amputees experience some of the same problems as transfemoral amputees, due to the similar complexities associated with the movement of the elbow. This makes mimicking the correct motion with an artificial limb very difficult. In the prosthetic industry a trans-humeral prosthesis is often referred to as a "AE" or above the elbow prothesis.
Current Technology/Manufacturing
In recent years there have been significant advancements in artificial limbs. New plastics and other materials, such as carbon fiber, have allowed artificial limbs to be stronger and lighter, limiting the amount of extra energy necessary to operate the limb. This is especially important for transfemoral amputees. Additional materials have allowed artificial limbs to look much more realistic, which is important to transradial and transhumeral amputees because they are more likely to have the artificial limb exposed.[8]
In addition to new materials, the use of electronics has become very common in artificial limbs. Myoelectric limbs, which control the limbs by converting muscle movements to electrical signals, have become much more common than cable operated limbs. Myoelectric limbs allow the amputees to more directly control the artificial limb. Computers are also used extensively in the manufacturing of limbs. Computer Aided Design and Computer Aided Manufacturing are often used to assist in the design and manufacture of artificial limbs.[8]
Most modern artificial limbs are attached to the stump of the amputee by belts and cuffs or by suction. The stump usually fits into a socket on the prosthetic. The socket is custom made to create a better fit between the leg and the artificial limb, which helps reduce wear on the stump. The custom socket is created by taking a plaster cast of the stump and then making a mold from the plaster cast. Newer methods include laser guided measuring which can be input directly to a computer allowing for a more sophisticated design.
One of the biggest problems with the stump and socket attachment is that there is a large amount of rubbing between the stump and socket. This can be painful and can cause breakdown of tissue.[9]
Artificial limbs are typically manufactured using the following steps:[8]
- Measurement of the stump
- Measurement of the body to determine the size required for the artificial limb
- Creation of a model of the stump
- Formation of thermoplastic sheet around the model of the stump – This is then used to test the fit of the prosthetic
- Formation of permanent socket
- Formation of plastic parts of the artificial limb – Different methods are used, including vacuum forming and injection molding
- Creation of metal parts of the artificial limb using die casting
- Assembly of entire limb
Emerging Technology
There are several areas of technology that have advanced significantly in recent years and are showing considerable potential. Robotic limbs and direct bone attachment are two new technologies that have made tremendous gains recently.
Robotic Limbs
Advancements in the processors used in myoelectric arms has allowed for artificial limbs to make gains in fine tuned control of the prosthetic. The Boston Digital Arm is a recent artificial limb that has taken advantage of these more advanced processors. The arm allows movement in five axes and allows the arm to be programmed for a more customized feel.[11]
Recently the i-Limb hand, invented in Edinburgh, Scotland, by David Gow has become the first commercially available hand prosthesis with five individually powered digits. The hand also possesses a manually rotatable thumb which is operated passively by the user and allows the hand to grip in precision, power and key grip modes. Raymond Edwards, Limbless Association Acting CEO, is the first amputee to be fitted with the i-LIMB by the National Health Service in the UK[12]. The hand, manufactured by "Touch Bionics"[13] of Scotland (a Livingston company), went on sale on 18 July 2007 in Britain.[14]. It was named alongside the Super Hadron Collider in Time magazine's top 50 innovations [15].
Another neural prosthetic is Johns Hopkins University Applied Physics Laboratory Proto 1. Besides the Proto 1, the university also finished the Proto 2 in 2010. [16]
Targeted muscle reinnervation (TMR) is a technique in which motor nerves which previously controlled muscles on an amputated limb are surgically rerouted such that they reinnervate a small region of a large, intact muscle, such as the pectoralis major. As a result, when a patient thinks about moving the thumb of his missing hand, a small area of muscle on his chest will contract instead. By placing sensors over the reinervated muscle, these contractions can be made to control movement of an appropriate part of the robotic prosthesis.[17][18]
An emerging variant of this technique is called targeted sensory reinnervation (TSR). This procedure is similar to TMR, except that sensory nerves are surgically rerouted to skin on the chest, rather than motor nerves rerouted to muscle. The patient then feels any sensory stimulus on that area of the chest, such as pressure or temperature, as if it were occurring on the area of the amputated limb which the nerve originally innervated. In the future, artificial limbs could be built with sensors on fingertips or other important areas. When a stimulus, such as pressure or temperature, activated these sensors, an electrical signal would be sent to an actuator, which would produce a similar stimulus on the "rewired" area of chest skin. The user would then feel that stimulus as if it were occurring on an appropriate part of the artificial limb.[17]
Recently, robotic limbs have improved in their ability to take signals from the human brain and translate those signals into motion in the artificial limb. DARPA, the Pentagon’s research division, is working to make even more advancements in this area. Their desire is to create an artificial limb that ties directly into the nervous system.[19]
Cosmesis
 |
 |
|
|
A French mutilé in 1918 wearing a mask provided by the American Red Cross (left) and without mask (right)
|
||
Cosmetic prosthesis has long been used to disguise injuries and disfigurements. With advances in modern technology, cosmesis, the creation of lifelike limbs made from silicone or PVC has been made possible. Such prosthetics, such as artificial hands, can now be made to mimic the appearance of real hands, complete with freckles, veins, hair, fingerprints and even tattoos. Custom-made cosmeses are generally more expensive (costing thousands of US dollars, depending on the level of detail), while standard cosmeses come ready-made in various sizes, although they are often not as realistic as their custom-made counterparts. Another option is the custom-made silicone cover, which can be made to match a person's skin tone but not details such as freckles or wrinkles. Cosmeses are attached to the body in any number of ways, using an adhesive, suction, form-fitting, stretchable skin, or a skin sleeve.
Cognition
Unlike neuromotor prostheses, neurocognitive prostheses would sense or modulate neural function in order to physically reconstitute or augment cognitive processes such as executive function, attention, language, and memory. No neurocognitive prostheses are currently available but the development of implantable neurocognitive brain-computer interfaces has been proposed to help treat conditions such as stroke, traumatic brain injury, cerebral palsy, autism, and Alzheimer's disease.[20] The recent field of Assistive Technology for Cognition concerns the development of technologies to augment human cognition. Scheduling devices such as Neuropage remind users with memory impairments when to perform certain activities, such as visiting the doctor. Micro-prompting devices such as PEAT, AbleLink and Guide have been used to aid users with memory and executive function problems perform activities of daily living.
Direct Bone Attachment / Osseointegration
Osseointegration is a new method of attaching the artificial limb to the body. The stump and socket method can cause significant pain in the amputee, which is why the direct bone attachment has been explored extensively. The method works by inserting a titanium bolt into the bone at the end of the stump. After several months the bone attaches itself to the titanium bolt and an abutment is attached to the titanium bolt. The abutment extends out of the stump and the artificial limb is then attached to the abutment. Some of the benefits of this method include:
- Better muscle control of the prosthetic.
- The ability to wear the prosthetic for an extended period of time; with the stump and socket method this is not possible.
- The ability for transfemoral amputees to drive a car.
The main disadvantage of this method is that amputees with the direct bone attachment cannot have large impacts on the limb, such as those experienced during jogging, because of the potential for the bone to break.[9]
Prosthetic enhancement
In addition to the standard artificial limb for everyday use, many amputees or congenital patients have special limbs and devices to aid in the participation of sports and recreational activities.

Within science fiction, and, more recently, within the scientific community, there has been consideration given to using advanced prostheses to replace healthy body parts with artificial mechanisms and systems to improve function. The morality and desirability of such technologies are being debated. Body parts such as legs, arms, hands, feet, and others can be replaced.
The first experiment with a healthy individual appears to have been that by the British scientist Kevin Warwick. In 2002, an implant was interfaced directly into Warwick's nervous system. The electrode array, which contained around a hundred electrodes, was placed in the median nerve. The signals produced were detailed enough that a robot arm was able to mimic the actions of Warwick's own arm and provide a form of touch feedback again via the implant.[21]
In early 2008, Oscar Pistorius, the "Blade Runner" of South Africa, was briefly ruled ineligible to compete in the 2008 Summer Olympics because his prosthetic limbs were said to give him an unfair advantage over runners who had ankles. One researcher found that his limbs used twenty-five percent less energy than those of an able-bodied runner moving at the same speed. This ruling was overturned on appeal, with the appellate court stating that the overall set of advantages and disadvantages of Pistorius' limbs had not been considered. Pistorius did not qualify for the South African team for the Olympics, but went on to sweep the 2008 Summer Paralympics, and has been ruled eligible to qualify for any future Olympics.
The "Luke arm" is an advanced prosthesis currently under trials as of 2008.[22]
Cost
Transradial and transtibial prostheses typically cost between US $6,000 and $8,000. Transfemoral and transhumeral prosthetics cost approximately twice as much with a range of $10,000 to $15,000 and can sometimes reach costs of $35,000. The cost of an artificial limb does recur because artificial limbs are usually replaced every 3–4 years due to wear and tear. In addition, if the artificial limb has fit issues, the limb must be replaced within several months.[23] [24].
Jaipur Foot, an artificial limb from Jaipur, India, costs about US$ 40.
Low cost above knee prostheses often provide only basic structural support with limited function. This function is often achieved with crude, non-articulating, unstable, or manually locking knee joints. A limited number of organizations, such as the International Committee of the Red Cross (ICRC), create devices for developing countries. Their device which is manufactured by CR Equipments is a single-axis, manually-operated locking polymer prosthetic knee joint. [25] Aulie Devices Inc. produces prosthetic devices for harsh environments such as Vietnam. [26] In addition, a number of universities in the United States have begun to develop low cost poly-centric prosthetic knee joints claiming costs as low as $20. [27][28] Bloorview Research Institute in Canada has developed a low cost prosthetic knee joint (LC Knee) based on a single-axis mechanism composed of injection moldable polymers. Unlike other low cost devices, the prosthetic knee’s novel stance phase locking technology allows users to attain higher levels of function while maintaining stability. [29]

There is currently an open Prosthetics design forum known as the "Open Prosthetics Project". The group employs collaborators and volunteers to advance Prosthetics technology while attempting to lower the costs of these necessary devices. Visit their site at http://OpenProsthetics.org.
A plan for a low-cost artificial leg, designed by Sébastien Dubois, was featured at the 2007 International Design Exhibition award show in Copenhagen, Denmark. It would be able to create an energy-return prosthetic leg for US $8.00, composed primarily of fiberglass.[30]
See also
- Prosthetist
- Amputation
- Anaplastology
- Artificial organ
- Artificial knee
- Machine
- Cyborg
- Brain computer interface
References
- ↑ Eric Schremp involved in accident damaging nerves
- ↑ Accidents involving damage of nerves only requiring FES, as seen with Eric Schremp
- ↑ "Science, Medicine, and the Future: Artificial Limbs", BMJ, 29 September 2001. Retrieved 11 February 2007.
- ↑ 4.0 4.1 "History of Prostheses", University of Iowa, 5 June 2006. Retrieved 11 February 2007.
- ↑ 5.0 5.1 "Cairo toe earliest fake body bit", BBC News, 27 July 2007. Retrieved 27 July 2007.
- ↑ "Bronze single crown-like prosthetic restorations of teeth from the Late Roman period = Des restaurations par prothèses identiques à des couronnes en simple bronze de dents pendant la fin de la période romaine". Cat.inist.fr. http://cat.inist.fr/?aModele=afficheN&cpsidt=1557911. Retrieved 2009-11-03.
- ↑ OPnews The origins of De Soutter Medical
- ↑ 8.0 8.1 8.2 8.3 "Artificial Limb", How Products are Made, 2007. Retrieved 11 February 2007.
- ↑ 9.0 9.1 9.2 "Getting an Artificial Leg Up", Australian Broadcasting Corporation, 2000. Retrieved 11 February 2007.
- ↑ Physics: A First Course. "Connections, designing a better prosthetic leg"
- ↑ Recently the i-Limb hand, invented in Edinburgh, Scotland, by David Gow has become the first commercially available hand prosthesis with five individually powered digits. The hand also possesses a manually rotatable thumb which is operated passively by the user and allows the hand to grip in precision, power and key grip modes. "Advanced Signal Processing Dramatically Improves Capability of Artificial Limbs", SIGMO Technology, 2005. Retrieved 11 February 2007.
- ↑ "Bionic hand wins top tech prize". BBC News. 9 June 2008. http://news.bbc.co.uk/1/hi/sci/tech/7443866.stm. Retrieved 25 April 2010.
- ↑ http://www.touchbionics.com/professionals.php?section=5
- ↑ Highfield, Roger (31 May 2008). "Gripping stuff". The Daily Telegraph (London). http://www.telegraph.co.uk/motoring/2754644/Gripping-stuff.html. Retrieved 25 April 2010.
- ↑ http://current.com/items/89499345/bionic_hand_makes_top_inventions_list.htm
- ↑ Proto 1 and Proto 2
- ↑ 17.0 17.1 Kuiken TA, Miller LA, Lipschutz RD, Lock BA, Stubblefield K, Marasco PD, Zhou P, Dumanian GA (February 3, 2007). "Targeted reinnervation for enhanced prosthetic arm function in a woman with a proximal amputation: a case study". Lancet 369 (9559): 371–80. doi:10.1016/S0140-6736(07)60193-7. PMID 17276777.
- ↑ http://www.technologyreview.com/blog/editors/22730/
- ↑ Defense Sciences Office
- ↑ Serruya MD, Kahana MJ (2008). "Techniques and devices to restore cognition". Behav Brain Res 192: 149. doi:10.1016/j.bbr.2008.04.007. PMID 18539345.
- ↑ Warwick,K, Gasson,M, Hutt,B, Goodhew,I, Kyberd,P, Andrews,B, Teddy,P and Shad,A. “The Application of Implant Technology for Cybernetic Systems”, Archives of Neurology, 60(10), pp1369-1373, 2003
- ↑ "IEEE Spectrum: Dean Kamen's "Luke Arm" Prosthesis Readies for Clinical Trials". http://spectrum.ieee.org/biomedical/bionics/dean-kamens-luke-arm-prosthesis-readies-for-clinical-trials.
- ↑ "Cost of Prosthetics Stirs Debate", The Boston Globe, 5 July 2005. Retrieved 11 February 2007.
- ↑ [8]
- ↑ "ICRC: Trans-Femoral Prosthesis – Manufacturing Guidelines"
- ↑ "Aulie Devices Inc", 2006.
- ↑ "LEGS: Innovative, Low-Cost Prosthetic Limb Technology for the developing world", LeTournea University, 2009
- ↑ “$20 artificial knee for patients in the developing world”, Dan Stober, Stanford News Service, April, 2009.
- ↑ "Low-Cost Prosthetic Knee Joint" Bloorview Research Institute, LC Knee
- ↑ INDEX:2007 INDEX: AWARD
External links
- Chard Museum Display of James Gillingham's work on post WW1 artificial limbs.
- OandPCare.org has an extensive glossary of terms relating to artificial limbs, prostheses and the field of prosthetics
- National Amputee Centre — Information about artificial limbs
- O&PCare has a complete glossary relating to the field of prosthetics
- How Stuff Works : Biomechatronics - An overview of the field of biomechatronics, of which prosthetics is a part